Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
In a 3- to 4-page paper, address the following:
Explain the proposed solution you selected, how it addresses the major gap you identified in the current state workflow, and how it is related to operational efficiency.
Provide your future-state workflow model. The solution you would implement to address gap(s) in the current-state workflow should be clear within your new model. Be sure to copy/embed the actual image of your model, rather than just provide a link to the model.
Create a detailed use case of a real-world scenario that shows the steps of the future-state workflow you developed and discuss how it would be used in a real-world setting.
Outline the major steps and organizational changes that would be necessary to transition from the current state to the future-state workflow.
Explain one potential implementation strategy for the redesigned workflow that would be useful for this project. Justify the strategy’s appropriateness for your workflow and practice setting, as well as the thought process regarding this strategy.
Explain how organizational structure or culture can affect the long-term success of a project implemented to improve workflow.
Select 2–3 specific factors or issues and explain how they might impact the successful long-term implementation of a project. Identify at least one strategy for addressing each factor or issue you selected.
Support your workflow redesign by synthesizing and integrating at least two outside resources and two of the provided Resources. Include a reference list with APA-formatted citations of the resources you used.
Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
Workflow Redesign Part 1 (Gap Analysis Results)
The previous gap analysis focused on identifying inefficiencies in the workflow, defining medication administration, and assessing the input to the role of EHR in the identified issues. The goals included improving medication safety, optimizing EHR use, and reducing administration errors. The data was collected via direct observation and interviews. At the same time, an audit of the EHR logs revealed gaps in workflows such as the interaction of nurses with EHR, verification of medication and communication between nurse professionals and the pharmacists.
Gap Analysis Results (Summary)
The previous gap analysis identified several shortfalls with medication administration workflows. One of the identified and recurring issues was the medication administration delay, which resulted from challenges with the EHR systems user interface. Secondly, medication orders were required to be verified at diverse levels, including manual and time-consuming procedures. I.e. the pharmacists were required to cross-check the orders before they were approved. This practice delayed the process, especially when complex cases or patient-specific contraindications were being addressed. Secondly, the analysis found that the clinical decision support was underutilized. This is whereby, despite an inbuilt system within the EHR for safety alerts, most workers either bypassed or ignored the CDS tool. This worker’s behavior of bypassing the CDS tool increased the chances of medication errors being recorded (Ozkaynak et al., 2022).
Regarding the gaps identified, they align with the goals set, such as reducing medication errors and improving the timeliness of medication administration. Nevertheless, some additional issues were identified in the analysis, including a lack of effective workforce training regarding utilization of the EHR due to poor system design, which failed to foster a streamlined workflow.
ORDER A HUMAN-WRITTEN, PLAGIARISM-FREE PAPER HERE
Linking the Identified Issues to EHR & Meaningful Use Objectives
The issues identified in the conducted analysis were very closely identified with the meaningful stage II objectives, which, on their part, emphasized improving patient safety and ensuring timely medication administration. On the other hand, the EHR system’s shortfalls, including challenges in navigation and underutilization of its features, including the CDS tool, directly hindered the achievement of the objectives identified. For example, the inability of the workers to effectively use the CDS tool undermined the effectiveness of the clinical decision support, resulting in avoidable medication errors. Secondly, the use of meaningful use advocated for medication reconciliation to ensure medications were accurately administered; however, delays in order verification hindered this objective. More so, the findings also aligned with the broader target goal of ensuring patient-centered care is practiced and delivered, which is another objective. According to Zayas-Cabán et al. (2021), when healthcare professionals spend much time navigating the EHR system, it distracts their focus and ability to provide direct patient-focused care.
The Finalized/Updated Workflow Model
The updated workflow model will address the diverse inefficiencies identified earlier and in their previous analysis. Key changes or improvements would include a streamlined verification process, including an automated medication cross checking with relevant patient records, reducing redundant manual work (Lachman et al., 2020). This improvement would reduce the overall time nurses and pharmacists spend on verification process, resulting in faster medication delivery and overall organization and workers efficiency. Secondly, the updated workflow model would foster or enhance the use of CDS tools in the EHR system, reducing the risk of medication errors. The revised workflow will factor in and integrate workforce training on using diverse system tools, including the CDS, to motivate the workers to utilize the tools effectively in the best possible ways, reducing medication errors significantly (McGonigle & Mastrian, 2024). Finally, the refurbished system will include a nurse-pharmacist communication feature, allowing the two healthcare professionals to coordinate and address any issues arising from medication administration, i.e. discrepancies, and overall reduce delays. The messaging feature integrated into the EHR would also support teamwork and collaborative care delivery.
Expanding further on the refurnished workflow, the affected stakeholders would have their roles and responsibilities changed equally. In the refurbished workflow, the nurses will receive and verify the medication order. This is done through the EHR system and against patient records. They also administer the retrieved medication and documents. The system would, however, include prompts guiding the nurse through verification and safety checks, reducing the risks of omitting critical alerts. The previous workflow entailed manual cross-checking by the nurse on the medication orders, which resulted in delays; hence, the current system is automated.
The pharmacist’s role in the set-up entails reviewing and approving medication orders. He would also ensure any interaction with medication is flagged during the order review. In the previous workflow, the pharmacists experienced delays due to the complexity of medication cross-checking manually. This gap is addressed via the automation of some verification steps in the EHR system.
Lastly, there is the EHR system, which, in this case, plays the central role in ensuring the improvements are well integrated and in facilitating medication administration. Its functionality provides decision support by flagging potential errors and alerting the staff of discrepancies between orders and patient records. The previous overlooking or underutilization of CDS tools limited the overall potential of the system to prevent medication-related errors and safety concerns. With the revised workflow, there would be an emphasis and training on properly using the system and its diverse tools. This would ensure maximum leverage of the EHR system to the benefit of effective patient-based care Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results.
Conclusion
The gap analysis provided an indispensable foundation for improvement as it revealed different inefficiencies in medication administration workflow, some of which stemmed from poor use and underutilization of EHR tools. The revised workflow, however, addresses the identified issues via further workforce training on system usability and automation of medication verification process. the integrated changes in the workflow focus on enhancing the system’s efficiency and overall safety of the medication administration.
Gap Analysis Plan
One of the most challenging issues in the process of workflow in healthcare settings is ineffective and error-prone medication administration closely connected with the use of Electronic Health Records (EHR). It manifests in form of frequent drug errors, such as wrong dosages, wrong medications, and omissions. These are often compounded by poorly designed EHR systems that do not support the nursing staff in managing their tasks. This is directly related to Meaningful Use Objectives, mainly on improving patient safety and reducing medication errors. With the added emphasis of clinical decision support and medication reconciliation in Meaningful Use Stage 2 to make certain that medications are timely and appropriately provided, this really does seem like an area that needs major improvement.
Workflow Issue Analysis Using IOM Six Aims of Care
The medication administration workflow problem affects many dimensions of patient care identified in the IOM Six Aims of Care:
- Patient-centered care: the agitation in EHRs diverts a nurse away from their patients, therefore, less involvement of patients occurs, hence undermining the accuracy of such care.
- Timely manner: navigating through the EHR system takes time for nurses to complete medication orders, which may lead to late or missed doses that may compromise care.
- Effective: The integration of EHR in clinical workflows could either be effective or be an ineffective use of health information technology and, thus result in medication administration errors (Zayas-Cabán et al., 2021).
- Efficient: The current workflow makes nurses repeat steps. For example, cross-checking medication orders on multiple screens, which takes longer time meant for more constructive actions.
- Equitable: Patients with complex needs, or those in rural settings, can often experience poor outcomes, as the administration of medication is inconsistent, seeing that most EHR systems have no flexibility to adapt to these various needs of patients.
- Safe: The current workflow creates considerable risk for patients via its predisposition to medication errors. Automation through systems, such as the CDS tools part of the EHR, can be enlisted to help reduce these errors but go underutilized (Lachman et al., 2020).
Goals for the Gap Analysis
Objectives of this gap analysis include the following:
- To identify any inefficiencies or sources of error in the current workflow around medication administration.
- To discuss the current EHR system based on the Meaningful Use goals with respect to medication safety and clinical decision support.
- To establish actionable strategies in order to enhance workflow through EHR functionalities, optimizing them to timely, accurately, and efficiently administer medications.
Methods of Data Collection
The review of the issues with workflows will be done through direct observation, interviews with the staff, and auditing of the EHR data. Targets for direct observation will include nursing staff, pharmacists, and EHR personnel involved in the process of medication administration (Renjith et al., 2021). Precise tools for data collection will involve:
- Narrative Statements: It will involve direct observation of staff interaction with the EHR system with an aim of determining the points at which delays or errors are occurring Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results.
- Checklists: cross-reference the medication orders with records to monitor the accuracy and timeliness of administration.
- Interview questions: Include but are not limited to the following: “What’s most difficult for you when giving medications in the EHR system?” and “How does the interface of the system affect or impact your workflow?”
Minimizing Disruption and Avoiding Bias
To minimize disruptions and avoid bias, I will first be shadowing the staff during less busy hours so that disturbance due to data collection is minimal during the observations. Furthermore, to avoid biased views, I will ensure that observations and interviews are performed on a mixed sample of staff with regard to experience and different shifts. Also, I will seek more objective data provided by the EHR system in order to complement subjective observations and interviews and reduce the possible incidence of personal biases.
Data Recording, Quantification, and Analysis
Qualitative and quantitative data collection approaches shall be employed. The qualitative data shall include some narrative observations of workflow disruptions among other forms, while the quantitative ones will involve such metrics as average time to perform medication administration activities and frequency of medication errors (McGonigle & Mastrian, 2024). In completing the normalizing of the data, several sources must first be derived in order to initially provide base-line metrics through review of historical EHR logs cross-referenced with medication error reports. These will then provide baselines that identify variances and areas of improvement for workflow optimization. Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
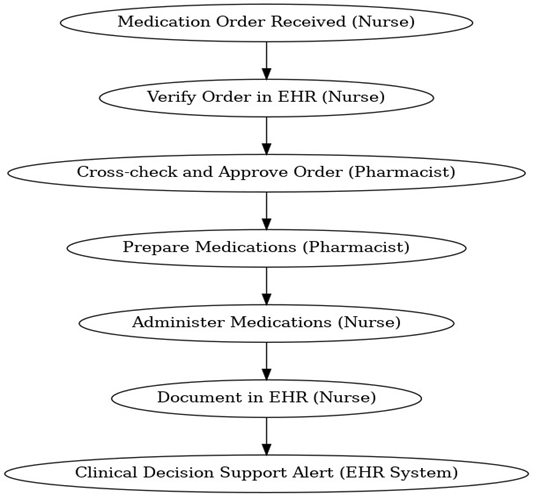
Current-State Workflow and Swimlane Diagram
The current work routine of medication administration includes multiple phases of the process. These include receiving medication orders, verification against EHR, retrieval of the medication, administration to patients, and recording in EHR (Ozkaynak et al., 2022). There are many stages with slow processing because it is not easy to navigate-need for manual cross-checking. Below is a swimlane diagram showing major stakeholders and their responsibilities.
- Nurse: Prepares and administers medications. They also document actions in the EHR.
- Pharmacist: Cross-checks and approves the orders that are related to medications in the EHR.
- EHR system: Provides medication order entry, patient allergy checks, and clinical decision support.
Conclusion
In a recap, this paper discusses a thorough analysis of how the current EHR system affects the workflow of medication administration, most especially with reference to Meaningful Use Objectives and IOM Six Aims of Care. With evidence from observation, interviews, and EHR metrics, recommendations that could enhance medication safety and foster the general efficiency of the workflow are outlined. These will help bridge the gaps in practice and subsequently improve patient outcomes, increase staff satisfaction, and reduce medication administration errors.
Workflow Redesign Part 2 and Finalized Course Project
In healthcare organizations, appropriate and smooth workflow and EHR implementations are crucial to minimize the threat of errors, enhance productivity, and promote high-quality care. Part 1 of the gap analysis revealed inefficiency, especially in the medication administration process, and highlighted poor EHR use. The established gaps: medication verification delays, low use of CDS, and no efficient communication between nurses and pharmacists require a more refined, automated approach. This paper presents a concept of a new, efficient workflow, a future state, an example of the application of the new workflow in real life, and how to get from the current state to the future one. Moreover, this paper discusses an implementation plan and considers the role of organizational culture in the long-term success of a project.
Proposed Solution and Relationship to Operational Efficiency
The new changes aim at the technology-based automated medication verification process, increased CDS tool utilization, and effective nurse-pharmacist collaboration. These changes are Meaningful Use Objectives, patient safety, medication reconciliation, and timely administration of medications (Zayas-Cabán et al., 2021). The proposed solution helps fill the above gaps by eliminating the need for manual data manipulation and introducing training for CDS tools. Also, the new workflow will include a communication component integrated into the EHR to support communication between the nurses and pharmacists in real time.
This simplified approach will enhance operation effectiveness by shortening the time necessary for confirmation, increasing the rate of medication delivery, and decreasing the rate of medication mistakes due to enhanced EHR functions. Research has also indicated that EHRs contain much of the same information, and efforts made to eliminate duplication and improve EHR utilization in clinical environments lead to increased patient safety and improved care (McGonigle & Mastrian, 2024). The redesigned workflow also allows the nursing staff to spend more time on related patient activities, increasing both efficiency and satisfaction. Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
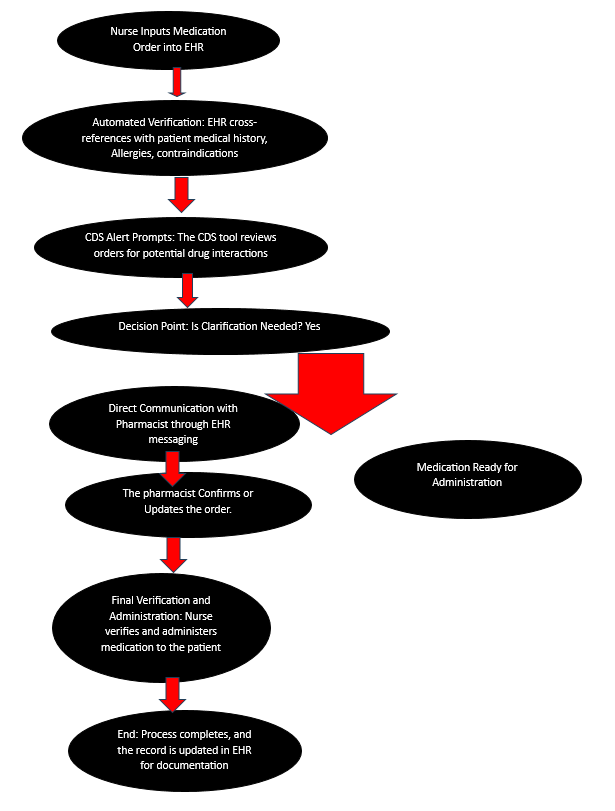
Future-State Workflow Model
The future-state workflow eliminates many manual verification processes and integrates workflow steps within the EHR system.
- Medication Order Verification: The nurse enters medication orders into the EHR, which checks them for safety, allergies, or even the dosage of the particular medication for the specific patient.
- Automated CDS Integration: The EHR will remind the nurse to view alerts from the CDS tool used in nursing practice. The system will prompt a confirmation to review before proceeding with the safety warning generated by CDS to catch the staff’s attention.
- Nurse-Pharmacist Communication: If there are any variations or concerns, a message communication tool integrated into the EHR will help promptly contact the other specialist, omitting communication delays noticed with basic paper and pen coordination.
This future-state model leads to improved workflow and more integrated nurse-pharmacist interactions. It eliminates unnecessary steps and delays and increases the reliability of medication administration.
Real-World Use Case: Future-State Workflow in Action
Think about a situation when a nurse gives medication to a patient with several chronic conditions. In the current workflow, the nurse will have to check every medication manually, which takes much time, and often has to discuss with the pharmacist if questions need to be answered. In the new design, the nurse enters the medication order into the EHR, and the system immediately cross-checks it with the patient’s record, highlighting any contraindications (Goucher, 2023). The CDS tool alerts the nurse that there might be an interaction with a prescribed drug, and the nurse affirms this alert in the EHR. If there is any confusion, the nurse can communicate with the pharmacist through the integrated EHR communication feature and always get an almost immediate response, which clears up any confusion immediately. By integrating these functionalities, the redesigned workflow allows the nurse to administer the medication within a few minutes, promoting safer and more efficient patient care.
Steps and Organizational Changes for Transition
According to Goucher (2023), To transition from the current state to the future-state workflow, several organizational adjustments and steps are necessary:
- System Enhancements: An upgrade of the EHR system to support the functions of automated verification and a CDS prompt, in addition to incorporating the embedded communication feature.
- Training Programs: Staff will need to attend seminars on using new EHR features, specifically the CDS alert. This training will, therefore, center on a new interface, CDS tools, and communication between nurses and pharmacists.
- Pilot Testing: However, the full-scale employment of the system will be preceded by pre-implementation in a limited setting, where staff can get acquainted with this new system and give feedback for further improvement.
- Ongoing Evaluation: After implementation, constant monitoring and evaluation should be conducted to check if the workflow is as planned planned, in case new problems arise due to changes in the staff’s working routine.
With these changes, the new workflow will reduce resistance and ensure that all staff can use the system to its maximum.
Implementation Strategy for the Redesigned Workflow
The implementation will, therefore, be done in phases, with the first phase being a pilot study in one healthcare facility department before a full implementation is done. This approach reduces interruption while the staff adjusts to the new changes in workflow as implemented by the redesign process. Pilots will assume real-world scenarios to identify problems that are likely to be encountered before widespread implementation. This strategy is suitable as it fits into the workflow, and the latter is oriented toward optimizing the execution of intricate procedures. Also, the findings reveal that phased implementations with feedback loops enhance the transition barriers and maximize the probability of adoption (Thieme et al., 2024).
Impact of Organizational Structure and Culture on Project Success
The impact of changes in the healthcare organization’s framework is highly dependent on the organizational structure and culture since workflow improvement is based on collaboration and communication. Two potentially modifiable barriers to long-term success are resistance to change and staff training on technology (Thieme et al., 2024).
Resistance to Change
There is always a standard practice in healthcare facilities, and changing this practice may meet some resistance, especially if it comes with the impression of creating more work. Its leadership can facilitate a clerical, information-sharing system that welcomes employee feedback and listens to complaints in frequent meetings. Very often, people only accept change if they are involved in the planning and implementation of the change.
Staff Training and Adaptation to Technology
The EHR’s CDS tools and communication features need training for their practical application. Otherwise, the staff will refrain from using the functions to increase safety levels. To this end, training programs focusing on the new workflow’s advantages will enable staff to identify the value addition (Thieme et al., 2024). Besides, the development of flow training and support tools means that new and experienced employees can successfully apply the changes in the working process (Goucher, 2023).
These strategies will help promote communication and structured training, which in turn will help foster a culture of innovation and a more ready acceptance of change.
Conclusion
Altogether, the suggested changes to the workflow in an outpatient clinic cover and meet the gaps and challenges identified during the initial gap analysis: the change from paper forms to electronic ones, higher usage of CDS, and better coordination between the clinic’s nurses and pharmacists. The future-state model shows an optimized process map with evidence from pilot testing, implementation phases, and strategy to address resistance to change. The new plan helps achieve operational effectiveness and Meaningful Use Objectives and promotes a patient-centric model that increases staff morale and patient outcomes. When implemented correctly and backed up by the proper training and a positive organizational culture, the new workflow can last for a long time, reducing the occurrence of medication errors and promoting substantive, safe healthcare practices. Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results
References
Goucher, M. C. (2023). A Nursing Workflow Process Change to Improve Medication Administration (Doctoral dissertation, Aspen University).
Lachman, P., Batalden, P., & Vanhaecht, K. (2020). A multidimensional quality model: an opportunity for patients, their kin, healthcare providers and professionals to coproduce health. F1000Research, 9. https://doi.org/10.12688%2Ff1000research.26368.3
McGonigle, D., & Mastrian, K. (2024). Nursing informatics and the foundation of knowledge. Jones & Bartlett Learning.
Ozkaynak, M., Unertl, K., Johnson, S., Brixey, J., & Haque, S. N. (2022). Clinical workflow analysis, process redesign, and quality improvement. In Clinical informatics study guide: Text and review (pp. 103-118). Cham: Springer International Publishing. https://doi.org/10.1007/978-3-030-93765-2_8
Renjith, V., Yesodharan, R., Noronha, J. A., Ladd, E., & George, A. (2021). Qualitative methods in health care research. International journal of preventive medicine, 12(1), 20. https://www.ijpvmjournal.net
Thieme, A., Rajamohan, A., Cooper, B., Groombridge, H., Simister, R., Wong, B., … & Jacob, J. (2024). Challenges for Responsible AI Design and Workflow Integration in Healthcare: A Case Study of Automatic Feeding Tube Qualification in Radiology. arXiv preprint arXiv:2405.05299.
Zayas-Cabán, T., Haque, S. N., & Kemper, N. (2021). Identifying opportunities for workflow automation in health care: lessons learned from other industries. Applied Clinical Informatics, 12(03), 686-697.
Zayas-Cabán, T., Marquard, J., & Ozkaynak, M. (2021). It is essential to understand the role of EHRs in workflow optimization and patient safety. Healthcare Quality Management Journal, 15(4), 97-109. Workflow Redesign Part 2 and Finalized Course Project – Gap Analysis Results